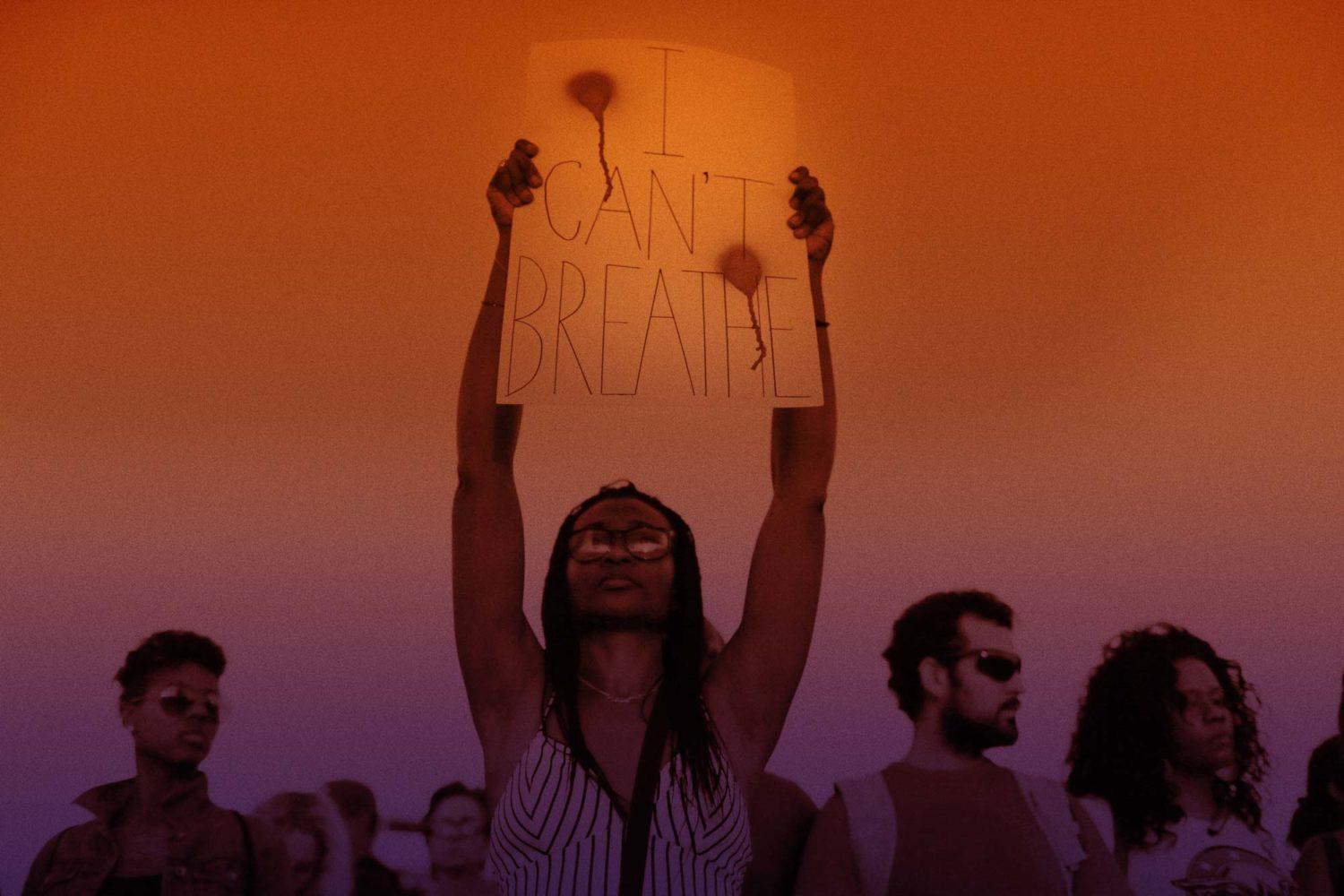
Why Is New York Still Paying Eric Garner’s Killer Six Figures?
Daniel Pantaleo remains with the NYPD four years after Garner’s death.
July marked the fourth anniversary of Eric Garner’s death. The city of New York is still paying NYPD officer Daniel Pantaleo—the man who put Eric Garner in a chokehold—six figures. The NYPD Patrol Guide prohibits chokeholds and states “excessive force will not be tolerated. [Officers] who use excessive force will be subject to Department discipline, up to and including dismissal.” Pantaleo’s employment isn’t completely surprising: In March, BuzzFeed published an investigation that showed over 300 NYPD officers who committed fireable offenses, including excessive force, were not fired.
Mayor Bill de Blasio claims that he has been waiting for the Department of Justice (DOJ), at their request, to finish their investigation into whether the DOJ will file criminal civil rights charges against Pantaleo. Ultimately, it’s the NYPD commissioner’s decision to discipline or fire officers—and the commissioner works for the mayor. On July 16, 2018, the NYPD released a letter sent from its legal department to the DOJ, saying that the police department would proceed with disciplinary hearings if they did not hear from the government by the end of August. But in a statement sent to news outlets, the DOJ said it had given the city the green light to move forward on disciplinary charges back in the spring.
In a recent press conference with the mayor, police Commissioner James O’Neill said Lawrence Byrne, who was a deputy commissioner until the end of last month, “was not informed of that. This is something that we’ve been following very closely obviously for years. He’s had many discussions with DOJ and never at any point prior to a couple of weeks [ago] did they say it was OK to move forward.” On July 20, the Civilian Complaint Review Board, the city’s police oversight agency that can investigate NYPD misconduct claims, filed disciplinary charges against Pantaleo and will prosecute the case in a departmental trial.
For Eric Garner’s family, the letter (signed by Byrne) was nothing more than a political spectacle. “[The NYPD] letter and the Justice Department response shows that the excuse that de Blasio and the NYPD have been using for not holding officers accountable is just that: a political excuse,” Gwen Carr, Garner’s mother, said in a statement released the next day. “In fact, DOJ’s response makes very clear that there is nothing stopping the NYPD from acting immediately to discipline officers and there’s no reason to wait until September, like NYPD’s letter laid out.” On July 25, Carr confronted de Blasio at a town hall in Staten Island and accused the de Blasio administration of blocking accountability and playing political games; she also asked him to discipline all the NYPD officers who were at the scene. Mayor de Blasio responded: “I respect the NYPD’s internal disciplinary process. There is due process; it is immediately beginning, we made that very clear.” He added that only two officers will face discipline: Pantaleo and Sgt. Kizzy Adonis.
Jennifer Laurin, a law professor at University of Texas who studies civil rights litigation, said the DOJ might have asked the NYPD to delay the disciplinary hearings for legal reasons. Specifically, the DOJ most likely doesn’t want any previous witness statements to contradict their own (since that can result in witnesses being impeached). But Laurin noted: “The DOJ can’t compel the NYPD to not do an internal investigation,” and added that, “the time that the NYPD has now waited to conduct its own investigation obviously, itself, can complicate that investigation,” because the police may no longer be able to track down witnesses.
For police brutality activists and Eric Garner’s family members, four years is way too long for de Blasio to wait when he has the power to fire Daniel Pantaleo. And Pantaleo’s future disciplinary hearing does not absolve de Blasio of failing to hold all the officers at the scene accountable.
“Here’s the reality: in the past four years, Mayor de Blasio and the NYPD could have acted at any time to deliver real accountability for Eric Garner’s killing by firing the officers who murdered him, failed to provide aid or intervene, tried to cover it up, and engaged in related misconduct,” Loyda Colon, co-director of Justice Committee and a spokesperson for Communities United for Police Reform, told The Appeal in an email. “But Mayor de Blasio and the NYPD have played games and used delay tactics every step of the way.” Colon called on de Blasio to stop the “blatant cover-up,” make Pantaleo and Adonis face disciplinary charges and then fire them immediately, and release the names of all the officers involved in Garner’s death.
“Mayor de Blasio has not lived up to his campaign promises of reforming the NYPD and making it more transparent and accountable to impacted communities,” Colon said. “Make no mistake: If he doesn’t make this right fast, his mayoral legacy will be tainted by his failure to hold police accountable, and the fact that a major NYPD cover-up of police misconduct in the killing of Garner happened on his watch.”
