‘No Shower, Wearing Diapers, Laying There For So Long’
Lawsuits that challenge mental healthcare and medical care for incarcerated people advance in Illinois.

On Dec. 21, 2015, Molly, then 23 years old, climbed the fence of Logan Correctional Center in Lincoln, Illinois, where she had been incarcerated since 2013. (To protect Molly’s identity, only her first name is being used.)
“I’m not trying to escape, I just wanted to cut myself,” she told the officers, according to a disciplinary report. She used the razor wire from the fence to cut her arm.
She was pepper sprayed and charged with disobeying a direct order to come down. Her punishment was one month of restricted recreation.
“I was a cutter before I went to prison, but it wasn’t that bad,” Molly, who was released earlier this year, told The Appeal. “But when I got to prison, it just spiraled out of control.”
Mental healthcare, as well as medical and dental care, for Illinois prisoners have been the subject of two class-action lawsuits against the Illinois Department of Corrections (IDOC)—Rasho v. Baldwin and Lippert v. Baldwin, filed in 2007 and 2010. Taken together, the suits paint a bleak picture of care for the bodies and minds of Illinois prisoners.
Most healthcare inside the state’s prisons is provided by Wexford Health Sources, which in 2011 was awarded a 10-year contract with the IDOC, worth more than $1.36 billion, according to a Wexford press release.
In 2016, the plaintiffs and the IDOC entered into a settlement agreement in Rasho v. Baldwin, in which the IDOC agreed to implement a wide range of reforms to improve its mental healthcare system. But on Oct. 30, U.S. District Judge Michael M. Mihm agreed with the plaintiffs that the IDOC has continued to provide inadequate care. He granted a permanent injunction, requiring the IDOC to comply with the settlement agreement and the U.S. Constitution, starting with submitting a plan detailing how it will do so.
“It is clear mentally ill inmates continue to suffer as they wait for the IDOC to do what it said it was going to do,” Mihm wrote in his order. “The Court cannot allow this to continue.”
Mihm found that, although some improvements had been made since the initial settlement, the IDOC remains “deliberately indifferent” to the needs of the more than 12,000 prisoners who are mentally ill.
When it comes to “medication management, mental health treatment in segregation, mental health treatment on crisis watch, mental health evaluations, and mental health treatment plans,” he wrote, the agency’s conduct defies the constitutional prohibition against cruel and unusual punishment. There are also “systemic and gross deficiencies in the staffing of mental health providers,” according to his order.
Alan Mills, executive director of Uptown People’s Law Center, said Mihm’s ruling was a “very important step.” Uptown People’s Law Center filed the suit with Equip for Equality, as well as Mayer Brown and Dentons, two global law firms.
“This is the judge saying, ‘You are violating the Constitution. You are actually harming people. You have to fix it,’” Mills told The Appeal.
In November, the defendants submitted a four-page plan on how to comply with the order, but it was criticized as inadequate by plaintiffs, who proposed their own more detailed plan.
The Court cannot allow this to continue.
Hon. Michael M. Mihm U.S. District Judge
On Dec. 17, Mills is scheduled to go to trial in Lippert v. Baldwin, also brought by Uptown People’s Law Center and Dentons, as well as the ACLU of Illinois. A report by the second court-appointed expert in that case, released in November, documented negligent and incompetent healthcare for the state’s prisoners.
When asked to describe the medical care for people inside Illinois prisons, Mills told The Appeal: “Deadly. We’re killing people.”
Self-harm and solitary confinement
While incarcerated, Molly compulsively harmed herself. She inserted objects, like paper clips, into her arms, and put feces and urine in her cuts, according to her prison records.
On July 20, 2014, Molly spat at an officer and used her toilet to flood her cell and the wing. The report documenting this episode includes the following note, apparently written by a mental health provider within the prison: “This offender has a chronic and pervasive, severe mental illness complicated by developmental delays that result in inappropriate and impulsive acting out with certain IDOC staff … extensive segregation time would be detrimental to her mental status and interfere with mental health treatment.”
She was given six months in segregation. Segregation, also known as solitary confinement, restricts prisoners to their cells for at least 22 hours a day.
“It kept getting worse and worse for me and I kept [being accused] of staff assaults. … I wasn’t in the right state of mind,” Molly said. “Just put me in that place and I just change. I’m not the same person anymore.”
In September 2014, when she was found with a torn sheet with the ends tied together and around her neck, she was placed on suicide watch and punished with one month of day-room restriction, which means she could not go to the day room where prisoners socialize together, according to her prison records.
As long as the baseline is punitiveness—how bad can we make this—then you’re never actually going to get people better.
Alan Mills Uptown People’s Law Center
On July 18, 2015, she damaged an outlet in the prison to remove the wire so she could cut herself with it. She was charged with “damage or misuse of state property.”
“I know I did it to myself, but I wasn’t in my right state of mind,” said Molly, who has been diagnosed with borderline personality disorder, bipolar 1, and post-traumatic stress disorder, according to her medical records.
During another episode of self-harm in 2015, officers demanded she “give up the object” she was cutting herself with, according to an incident report. She refused, was placed in restraints, charged with disobeying a direct order, and punished with a month in segregation.
“They would leave me in restraints with a dirty diaper for like six to 12 hours,” Molly said. “No shower, wearing diapers, laying there for so long.”
‘A very punitive system’
As a result of the settlement agreement in 2016, reforms have been made, including the construction of residential treatment units and changes to segregation policies, according to a brief from the Illinois attorney general’s office outlining the defendants’ arguments. For instance, the office says, if a patient with a serious mental illness commits an infraction that could lead to segregation, a mental health professional reviews the case and can recommend no time or reduced time in segregation.
The AG’s office, which is representing the IDOC in both civil suits, referred The Appeal to the IDOC and to Wexford Health Sources for comment. Wexford referred The Appeal to the IDOC, which declined to comment on either case.
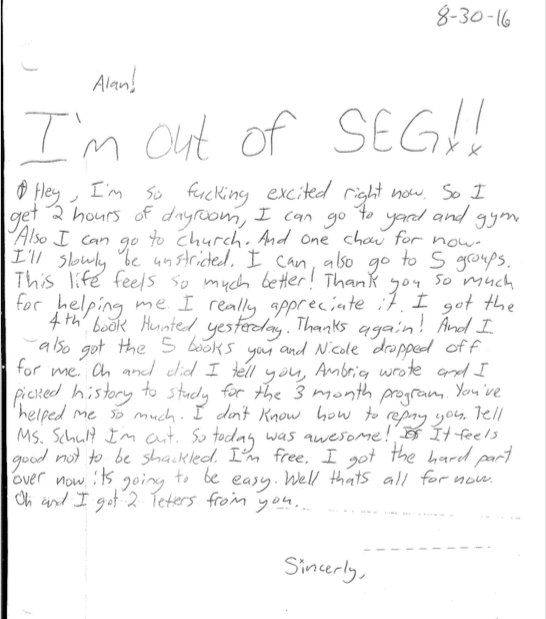
Molly’s care improved after the settlement agreement went into effect, according to Mills. She was released from a period of solitary confinement, and had access to more therapy groups, Mills said. “I’m out of SEG!!” Molly wrote to Mills in a letter dated Aug. 30, 2016. “It feels good not to be shackled. I’m free!”
But what Molly also needed was intensive inpatient care, which she never received, according to Mills. Her records show that she continued to harm herself.
On Jan. 7, 2017, Molly cut herself with a razor blade and was charged with “dangerous contraband.” She was disciplined with “two months C grade,” which meant she could not make or receive calls or go to commissary. The next month she was sentenced to a year in segregation after being accused of assaulting an officer.
Molly’s experience is not an anomaly, according to Mills. Despite some improvements, punitive responses to mental illness have continued in Illinois prisons, he said.
One patient at Stateville Correctional Center, for instance, was restrained continuously for at least nine months, since May 2017, “reportedly both for mental health and medical reasons,” the court-appointed monitor wrote in his second annual report for Rasho v. Baldwin, released in June. And more than 80 percent of the people in segregation inside Illinois prisons have mental illnesses, according to Mihm’s order.
When asked why so many people with mental illnesses were in segregation, Dr. Melvin Hinton, the IDOC’s chief of mental health services and addiction recovery services, testified at the preliminary injunction hearing that they “tend to have more behavioral issues, in part because of their mental illness.”
Mills said the cycle of punishing prisoners with mental illness and thus exacerbating their illness has to stop. “The way they treat people has to entirely change and be focused on getting people better rather than this sort of gloss of treatment on top of a very punitive system,” Mills said. “As long as the baseline is punitiveness—how bad can we make this—then you’re never actually going to get people better.”
‘Grossly and flagrantly unacceptable’
Some patients inside Illinois prisons suffer simultaneously because of the prisons’ mental and medical healthcare systems.
A 24-year-old man with mental illness died in October 2017 after he swallowed two plastic sporks and was denied medical care, according to the report of the second court-appointed expert in Lippert v. Baldwin. Even though a correctional officer witnessed the man ingest the sporks, the patient was not evaluated by a doctor. About two and half months later, the man, who had lost 33 pounds, told a nurse practitioner that he needed the sporks removed.
“The patient remained untreated and eventually lost 54 pounds and had repeated episodes of abdominal pain with an inability to eat without pain, nausea, and diarrhea,” the expert wrote.
When he was found unresponsive, he was sent to the hospital, where he died. His autopsy revealed his cause of death was esophageal perforation, caused by the swallowed sporks, according to the expert’s report.
Even though a correctional officer witnessed the man ingest the sporks, the patient was not evaluated by a doctor.
Lindsey Hess, the IDOC’s media administrator, declined to answer questions about this and other specific examples of medical neglect. “The Department cannot comment on the Lippert case at this time,” she wrote in an email to The Appeal.
The court-appointed expert reviewed 33 out of 174 deaths that occurred in 2016 and 2017, and found 19 were “preventable or possibly preventable.” Medical errors in these cases, the monitor wrote, were “so egregious that it would typically result in a peer review for possible reduction of privileges or referral to licensing boards for evaluation of sanction of their license.”
A prisoner in his 40s, for instance, deteriorated over several years as his undiagnosed and untreated HIV progressed, according to the report. His mobility became so limited that he needed a wheelchair. He was mistakenly given a medication that further decreased his white blood cell count. He was incontinent and confused.
The patient was finally sent to the hospital after suffering from severe hypoxemia (a low level of oxygen in the blood), abnormally low blood pressure, and tachycardia (an abnormally rapid heart rate). There he died of “AIDS related central nervous system disorder and disseminated systemic infection,” according to the expert’s report. He was severely malnourished, and his body was covered in pustular lesions.
Another death involved a patient on an anticoagulant and aspirin, which, the monitor wrote, “placed the patient at risk for life-threatening bleeding.” The patient was in the infirmary for three weeks, during which time he could not stand and was incontinent.
Despite bleeding from bruises that had developed, bleeding around his eyes, and blood in his stool, “no action was taken,” according to the expert’s report, which characterized the care as “grossly and flagrantly unacceptable.” When the patient began urinating blood, he was “incompetently treated for a presumed UTI [urinary tract infection],” the expert wrote.
After a nurse found the patient unresponsive, he was sent to the hospital where he was diagnosed with bleeding between his skull and brain. The court-appointed expert attributed these failings, in part, to a dearth of primary care trained physicians in Illinois prisons. “At least nine of 19 preventable or possibly preventable deaths were cared for by poorly trained physicians,” he wrote.
The problem is a structural one where all the incentives point in a negative direction in terms of providing quality, necessary care.
David Fathi ACLU National Prison Project
The Lippert v. Baldwin trial will feature testimony from people who have been denied care, Mills said. He hopes the court will issue an injunction, as in Rasho v. Baldwin, requiring specific changes from the IDOC, and that a monitor will be appointed to ensure the agency complies with the court’s order.
Permanent scars
Wexford has been accused of providing inadequate care for prisoners in several other states. In 2017, for instance, the Florida Department of Corrections announced it was terminating its contract with Wexford, calling the mental healthcare the company provided “life threatening.”
The deficiencies in care provided by Wexford illustrate the dangers of using a for-profit company to provide healthcare to a “disempowered and literally captive market,” said David Fathi, director of the ACLU National Prison Project.
“It’s not a problem of this company or that company,” he told The Appeal. “The problem is a structural one where all the incentives point in a negative direction in terms of providing quality, necessary care.”
Molly experienced that firsthand. She was released from prison this year, after serving about five years.
“The day I got out, my mom picked me up and it was just a really happy moment for me,” she said. “We just stay at home a lot and watch TV and spend time with each other.”
She colors, paints, and shops, she said. She doesn’t like to wear short-sleeved shirts in public because of the scars on her arms.
“Now I got scars,” Molly said. “I have scars all over my body.”
Although she is grateful to be home, she worries for those still inside and hopes that sharing her story can help them receive better care.
“I left my friends there. I feel really bad. I know what they’re going through,” Molly said. “Sometimes I look up their pictures [on the IDOC’s website] just so I can see them.”
Molly, now 26, said she is seeing a therapist and goes to her doctor’s appointments. “I’m being good.” But she fears returning to prison and said she often “walks on eggshells.”
“My doctors out of prison are so nice to me, I feel like it’s Christmas, birthdays, Easter, like all wrapped into one,” she said. “I’m just so happy to be out of that place. They really hurt me pretty bad on the inside and the outside. I don’t think I’ll ever go back.”
