Why Coronavirus in Jails Should Concern All of Us
New research shows that jails contribute to infectious disease deaths in the greater community.

This piece is a commentary, part of The Appeal’s collection of opinion and analysis.
Since Rikers Island jail complex reported its first case of coronavirus on Wednesday, the numbers there have risen rapidly: 38 people—staff and prisoners—have now tested positive for COVID-19. The New York City Board of Correction has repeatedly called on the city to immediately release from jail all people at high risk for coronavirus infection and rapidly decrease the jail population. Advocates and activists, too, have been pleading with state and local officials for days to release vulnerable people from jails, citing grave threats to the health of incarcerated people, staff, and the public.
This move can’t come soon enough. Substantial epidemiological research shows that mass incarceration raises contagion rates for infectious disease—both for people in jails, and for the community at large.
In our study recently published in the American Journal of Public Health, we found that increases in a county’s jail incarceration rate were associated with subsequent increases in county mortality rates between 1987 and 2016. In light of the coronavirus pandemic, we took another look at that data and found that infectious disease deaths contributed significantly to this increase. Specifically, increases in a county’s jail incarceration rate were associated with significant increases in county rates of infectious disease deaths.
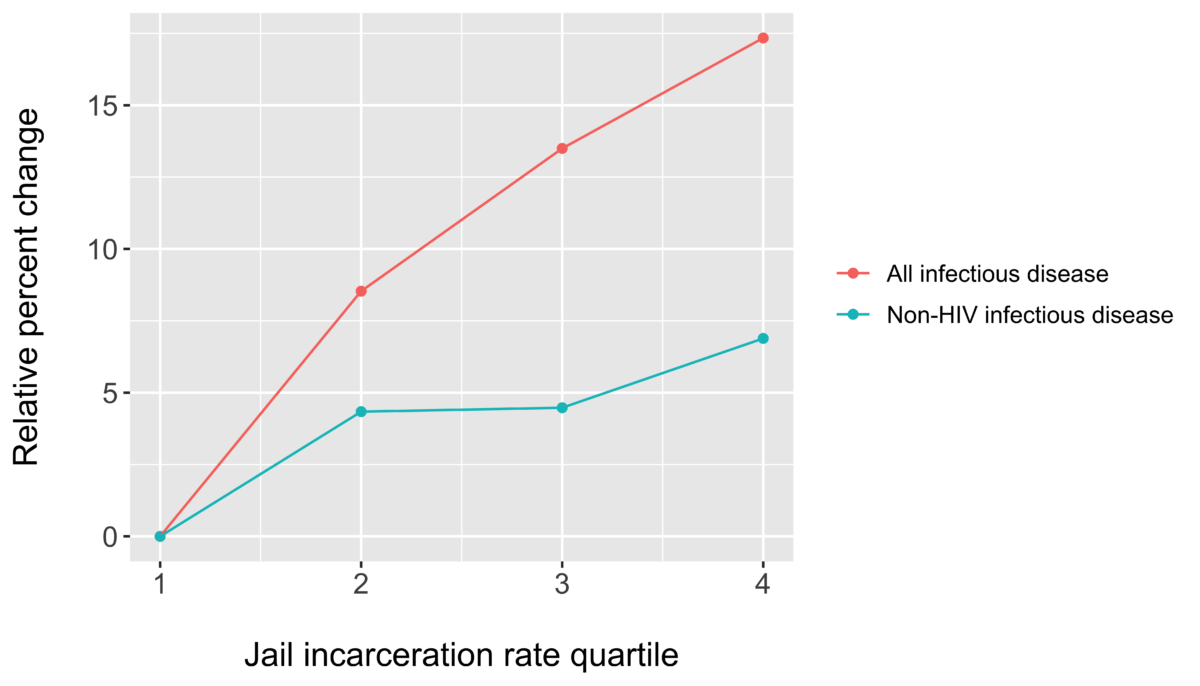
In this new analysis, we used data on 1,670 counties from 1987 to 2017. We ranked county jail incarceration rates into four equal quartiles (bottom 25 percent to top 25 percent), and found that if a county’s jail incarceration rate increased from the first to the second quartile, its mortality rate due to infectious disease increased by an alarming 9 percent. While death due to HIV drove much of this association, county mortality rates from other infectious diseases also rose. An increase in jail incarceration rate from the first to second quartile was associated with a 4 percent increase in the non-HIV infectious disease mortality rate.
So, even when we are operating under normal conditions, the association between jail incarceration and infectious disease mortality persists. This finding reflects deaths due to flu, pneumonia, and acute bronchitis, for example. This is empirical evidence that jail incarceration is most likely a driver of infectious disease deaths at the population level.
Jails and prisons are sites of disproportionate infectious disease rates. Incarcerated people suffer the most, but so do staff and communities, when jail conditions prevent people from following basic health precautions. A rapid reduction in the number of people in jails can help us slow the spread of coronavirus, “flattening the curve” of infection rates quickly enough to prevent the worst case scenario for public health.
The findings specific to the HIV epidemic are instructive, too. Researchers estimate that in 1997, near the height of the epidemic, 20 percent of all HIV-infected Americans had cycled in and out of a correctional facility at least once during the year. That meant the effects of inadequate healthcare in jails spilled over into the general population, with catastrophic public health consequences.
Why do jail incarceration rates contribute to community infectious disease mortality? Jails are short-term facilities and operate as revolving doors, aiding the spread of infectious disease not only within their confines, but also in the community. Jails can be dangerously overcrowded, ventilation is often poor, soap and cleaning supplies are often limited, and access to healthcare may be difficult or nonexistent. These conditions are antithetical to stopping the spread of infectious diseases like coronavirus.
Moreover, jails are not contained environments. In 2017, there were nearly 11 million admissions to jails across the country. Staff and visitors return to their homes every day. For prisoners, their average stay in jail is less than one month. At any given time, our country’s jails hold over 700,000 people, and the average weekly turnover rate is about 54 percent. Many of these individuals are held in unsafe conditions and then return to already vulnerable communities that have faced systematic disinvestment in social services and infrastructures.
In our analysis, which uses data from the Bureau of Justice Statistics and the Centers for Disease Control and Prevention, we compared counties to themselves over time. This way, we account for the fact that counties vary across the country and may not be comparable with each other.
Of course, our data is observational; we can’t rule out the possibility that something else may explain our results. However, we also took into account changes over time that may have explained the association, such as a county’s poverty rate and crime rate. Those factors did not explain away our findings. Our approach gives us confidence that our findings reflect generalized negative public health consequences of jail incarceration through the spread of infectious disease.
In response to coronavirus, daily civilian life has shifted significantly in an effort to slow the spread of disease and “flatten the curve.” At the beginning of the U.S. outbreak, the criminal legal system generally operated under business-as-usual protocols, jeopardizing the health of incarcerated individuals, correctional officers, and the general population at large.
Now, some jurisdictions are leading the way by holding mass plea hearings to reduce jail populations, halting incarceration for misdemeanor and traffic offenses, shifting to virtual court proceedings, and making plans to release the most vulnerable prisoners.
The coronavirus pandemic is a public health crisis unlike any we have seen in decades. It also exposes the inherent injustices of our criminal legal system, including the unconscionable number of people held in jails and prisons in inhumane conditions. The majority of people in jails are being held pretrial, many for misdemeanor charges. We must act now to release as many people from jails as we can, while recognizing that our system harms public health, even under normal circumstances.
Sandhya Kajeepeta, MSc, is a Ph.D. student in epidemiology at Columbia University.
Seth J. Prins, Ph.D. MPH, is assistant professor of epidemiology and sociomedical sciences at Columbia University.
