Political Report
Jail Deaths and the Elected Sheriff
Jail deaths happen with alarming regularity. The Badge probes the responsibility of sheriffs.
Jail deaths happen with alarming regularity. The Badge probes the responsibility of sheriffs.
This is part one of The Badge, a Political Report series on the powers and responsibilities of sheriffs.
Jails made headlines in 2015, when the 28-year-old Sandra Bland was arrested and placed in a Waller County, Texas, jail. She was unable to post bail, which was set at $5,000. Less than three days later, she was dead of an apparent suicide.
Such deaths happen with alarming regularity. A nationwide HuffPost study over one year identified an average of two fatalities per day. This first edition of The Badge, a new Political Report series on the powers of sheriffs, examines the problem of jail deaths and the responsibilities of sheriffs for the welfare of people in their custody.
Local jails house pretrial detainees who have not yet been found guilty of a crime and people serving short sentences. According to the National Sheriffs’ Association, 85 percent of local jails are run by sheriffs. In those spaces, it’s the responsibility of sheriffs to ensure that people have access to adequate healthcare and safe detention conditions.
This installment explores why jails are such dangerous places. It also reviews why the public does not know more about them, what policies could make jails safer, and why sheriffs often evade accountability.
The dangers of local jails
Jail deaths cover anything from suicides, deaths related to drug abuse disorder and prior medical conditions to childbirth, punitive or inadequate jail conditions and medical care, and assaults either by jail staff or other inmates. About a third of the jail deaths documented in the HuffPost investigation were suicides; as many occurred within days of arrest.
Jails can hinder access to adequate medical care
People taken to jail may suffer from pre-existing illnesses or substance abuse disorder, and given arrests’ sudden nature, they may find themselves without treatments and medications. Thus it can be of vital importance for jails to implement intake and detention procedures that inquire into these histories and hold—or release—people accordingly. Yet cases abound in which sheriff’s deputies were told of medical histories or psychiatric assessments but did not take that information into account.
Under Sheriff Randy Adams in Mineral County, Nevada, 27-year old Kelly Coltrain died while detained over traffic tickets. An investigation found that jail staff had failed to follow multiple protocols, for instance an intake requirement on how to detain people who share having a history of seizures. The investigation also found deputies denied her medical care for days and did not call paramedics after finding her unresponsive. After she told sheriff’s deputies that she needed care and medication, one deputy told her that, “You are incarcerated with us … you don’t get to go to the hospital when you want.” Here, as in other cases reviewed in this article, prosecutors declined to press charges.
When people experience healthcare needs in jail, jail staff decide whether to provide access to medical care and whether to move them to an infirmary or hospital. This lends itself to vastly inadequate treatment, whether out of malice, neglect, or insufficient resources. Deputies can ignore requests or delay response, at times until it’s too late. There are constant reports of preventable deaths of people who complained of health crises and exhibited signs of intense illness but were left untreated. Poor implementation of protocols such as regular welfare checks leaves emergencies and violent incidents unnoticed.
In addition, poor and rural counties are less likely to have adequate staff or medication on site, delaying treatment. “The more marginalized that you are, the more likely you are to not be believed, the more likely you are to get denied care,” attorney William Claiborne told the New York Times in January.
The Appeal has reported on a series of deaths under the watch of Sheriff Timothy Howard of Erie County, New York. India Cummings, a woman in a mental health crisis, was held more than two weeks in a cell without medical attention, eventually dying in a cell dirtied by her own urine. The state’s Commission of Correction wrote in a report that the care Cummings received was “so grossly incompetent and inadequate as to shock the conscience,” and that her death “should be ruled as a homicide due to medical neglect.” Twenty-four people have died while in Howard’s custody as of 2017, the latest data available. The county has faced lawsuits tying those death to lack of medical care.
Some sheriffs and other jail administrators contract with private healthcare providers whose quality of care has raised concerns. Recent New Yorker and WNYC investigations have documented complaints or lawsuits against for-profit companies that provide healthcare to many jails where there have been deaths. Statewide prison systems have faced similar questions regarding links between privatization and prison deaths.
Suicides are common in jail
For many people, the first days in jail cause mental and physical deterioration. Some may find themselves in sudden despair, away from community or family support. In these circumstances, poor screening when people are brought to jail and, later, poor monitoring or responsiveness can have disastrous consequences. Studies show that suicides are more likely in jail than prison.
When Massachusetts Attorney General Maura Healey called for an investigation into the high suicide rate in the Bristol County jails run by Sheriff Thomas Hodgson, she connected it to solitary confinement and poor access to services for people with mental illness, and to allegations of “unnecessarily harsh or unhealthy conditions.” The Prisoners Legal Services of Massachusetts, a prisoners rights group, has filed a lawsuit alleging that the sheriff forces people with diagnosed mental illnesses into solitary confinement. Hodgson called the lawsuit “frivolous.” In 2015, Brandon St. Pierre hang himself while in solitary confinement; a judge had warned that St. Pierre talked of suicidal thoughts.
Jails use solitary confinement and other punitive practices
Many other jails rely on solitary confinement, which worsens mental health problems and can lead to self-harm. Jail officials are known to resort to solitary confinement when people they detain are having mental health crises. Advocates have long fought its use.
In 2018, Sheriff Garry McFadden of Mecklenburg County, North Carolina, promised to eliminate it. Thus far, he has done so for teenagers. The sheriff of Florida’s Palm Beach County took the same step after a legal settlement.
Jail deaths have also been linked to other forms of abusive behavior, including beatings.
Then-Sheriff David Clarke of Milwaukee County, Wisconsin, ran a jail system decried for its abuses. In 2016, a man named Terrill Thomas died of dehydration after being cut off from water for seven days while being held in solitary confinement. An investigation found that water was denied other inmates as well, and faulted “an institutional practice of punitively shutting off water to unruly inmates.”
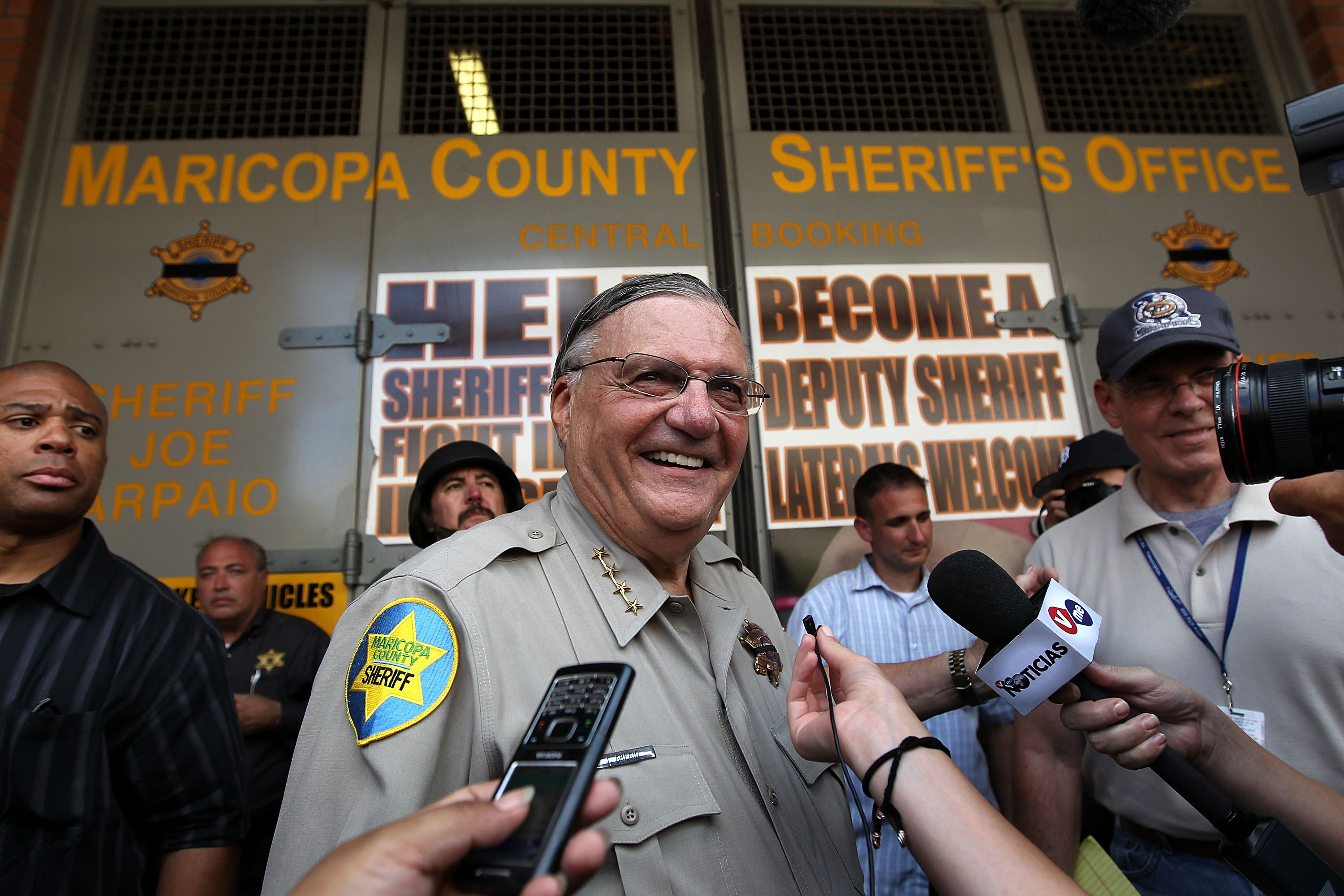
In 2018, The Appeal reported the death of 31-year old Michael Tyree in the hands of three officers in the context of wider confinement problems in Santa Clara County, California. And Maricopa County, Arizona, has reached a series of settlements over jail deaths that followed use of force by sheriff’s officers, such as the use of restraint chairs, under the tenure of former Sheriff Joe Arpaio. One such settlement was over Ernest Atencio, a man whom officers allegedly shot with a stun gun and beat after he refused to take off a shoe
Why do sheriffs remain in charge even when their jails are under fire?
Sheriffs’ power is wide but hard to track
It is difficult to force sheriffs to reform jails. As elected officials, they enjoy great discretion over how they run their department, and they cannot be removed by officials, such as governors and mayors, whose positions involve greater political contestation. Sheriffs’ powers are comparatively less known, which makes it harder for flawed behavior to register.
This is compounded by the jail system’s fragmented nature. That most jails are under the authority of county-level officials makes for inconsistent conditions and record keeping. In an investigation of New Jersey jails, WNYC reporters described a largely unregulated mishmash of reporting protocols, and erroneous and missing documents in county offices.
This also makes it difficult for watchdog groups to track and draw attention to violations.
There is no exhaustive database that documents reasons of death, in part because there are no consistent nationwide protocols. Some states have enacted stricter reporting requirements, however, and in response to a series of jail deaths, Utah lawmakers are considering legislation to tie funding for sheriff’s departments to compliance with transparency and disclosure regulations.
“At a very basic level, it’s doing public education,” Daisy Ramirez, the Orange County Jails Project Coordinator with the ACLU of Southern California, told me when I asked how to improve accountability. “It’s also about getting people in the media to talk about what’s happening in jails because, more often than not, the folks that have the most grievances about how the sheriff is operating are people that are currently in custody” and “encounter the most challenges when trying to draw attention to these issues.”
Systemic factors hinder meaningful investigations
Investigations can drag on or fall through the cracks. When Rebecca McCray tried to get information on the death of a 37-year old woman in the Multnomah County, Oregon, jail for the Appeal, she was bounced from the sheriff to the medical examiner to other officials. One official told her, “Twenty- to thirty-thousand people come through the jail every year, and some people unfortunately pass away.”
Some sheriffs enjoy greater authority than others to oversee and influence investigations. Most California counties have a sheriff-coroner system, which allows sheriffs to decide cause of death in cases involving their own officers. State legislation or county commissioners can end this dual role.
In San Joaquin County, California, two pathologists accused Sheriff Steve Moore of asking them to alter their findings to deflect responsibility. “He said to me that my opinion does not matter to him and does not mean anything in his office, … and that I must do what he orders me to do,” said the county’s former chief forensic pathologist. The county’s Board of Supervisors opted in 2018 to separate the coroner’s duties from the sheriff’s. Moore denied wrongdoing. He lost re-election in 2018
Ramirez told me that relationships between local officials are yet another obstacle to accountability even where investigations are not internal. “From 2010 to 2016, of the 48 people that lost their lives under the custody of the sheriff’s department, the DA’s office did not… criminally prosecute any staff,” she said of Orange County, California. “Given the close relationship between the sheriff’s department and the district attorney’s office, I think that that creates a level of mistrust among the public… I think it would be very powerful, in situations that would require it, to have outside agencies be the ones that are conducting these investigations.” New Jersey adopted a law this year that entrusts the state attorney general with investigating cases of people dying in custody. Ramirez also pointed to civilian oversight as a possible way to improve investigations, though she warned that such boards need “teeth to bring change and not just review reports.”
Jail guidelines are vague and unambitious
Sheriffs create their own rules about what constitutes adequate conditions. The Eighth Amendment of the U.S. Constitution forbids “cruel and unusual punishment,” but there are no clear national guidelines to which sheriffs must adhere. They determine whether to impose solitary confinement, for instance.
The National Center for Jail Operations does provide some criteria, though there is little in them on how to provide medical care or psychiatric assistance. But it is telling that in introducing this center’s purpose, the National Sheriffs’ Association (of which the center is a division) notes that it stems from a recognition that jails are “one of the most litigious and largest liability concerns a sheriff faces.” In 2018, the association advertised a webinar on suicide prevention with the headline “Avoiding Costly Lawsuits and Saving Money.”
Sheriffs can pursue bolder and more holistic goals. Policies that reduce detention, such as bail reform and cease-and-release programs that sheriffs can implement and expand, can shield people from jails’ poor conditions.
Idaho’s sheriffs association supported expanding Medicaid, linking improved public health with “keep[ing] people out of the jails.” And Ramirez pointed to how California’s county boards can “authorize the sheriff to release incarcerated folks… in lieu of confinement” as a sign sheriffs can “advocate for criminal justice reform.”